Cracking the code of itchy skin: A new way to diagnose and treat skin problems
Have you ever struggled with a skin condition that doctors found difficult to diagnose? Or perhaps you've been treated for a skin problem, but the treatment didn't work? Well, there’s some exciting news from a group of scientists who have been digging deep into the world of inflammatory skin diseases. They've come up with a clever new way to understand and treat these conditions, and it all comes down to something they call "immune modules".
What are Immune Modules?
Think of your immune system as a
complex network of pathways, each with its own job. These pathways can become
overactive and lead to inflammatory skin conditions like psoriasis, eczema
(atopic dermatitis), and lupus. The researchers have identified seven key
'immune modules', each representing a different pathway:
- Th17: Often seen in psoriasis.
- Th2: Common in eczema.
- Th1: Involved in conditions like lichen
planus.
- Type I IFNs: Related to lupus.
- Neutrophilic: Seen in conditions with lots
of neutrophils.
- Macrophagic: Related to macrophages.
- Eosinophilic: Linked to eosinophils.
The scientists found that by
looking at the activity of these modules in a skin biopsy, they could better
understand what was happening in an individual patient's skin.
A molecular map for skin diseases
The team created a
"molecular map" of inflammatory skin diseases, using these modules as
their guide. They took skin samples (biopsies) from patients with different
conditions and measured the activity of genes related to each module. They discovered
that each disease had its own distinct pattern of module activity. For
instance, psoriasis showed high activity in the Th17 module, while eczema
showed high activity in the Th2 module. This was like creating a fingerprint
for each disease, based on the activity of these modules.
This approach proved to be very
accurate in diagnosing various skin diseases, even those that are usually
tricky to identify. It was even better at classifying diseases than using all
the genes they measured or other standard methods. This molecular map also
worked well for diagnosing unusual cases like erythroderma (widespread skin
redness) and rashes where the cause was unknown.
The researchers didn't stop at
diagnosis. They also wanted to see if these immune modules could help guide
treatment decisions. Because each module corresponds to a specific immune
pathway that can be targeted with medication, they explored the possibility of
matching the dominant module in a patient's skin biopsy to the right treatment.
They looked at 80 patients who
were being treated for psoriasis, eczema or lichen planus, and they found that patients
who responded well to treatment had a module profile that matched the treatment
they were receiving. For example, if a patient with psoriasis had a
dominant Th17 module, they were more likely to respond to anti-Th17
medications. However, some patients were not responding because their module
profile did not match the treatment they were given. And of those who were not
responding to treatment, many had mismatched profiles, which were changed
according to the new model to achieve success.
Furthermore, they discovered that
in some patients, the dominant module in their skin changed under treatment,
causing them to stop responding. By identifying the new dominant module, they
were able to switch to a more effective treatment. This module-based approach
not only improved treatment responses but also helped to understand why some
treatments fail.
What does this mean for you?
This research is a big step
forward for people with inflammatory skin diseases. It suggests that:
- More accurate diagnoses are possible: Using
module-based profiling, doctors can diagnose conditions more accurately,
even when symptoms are confusing.
- Treatments can be tailored: By matching a
patient's dominant immune module to a targeted therapy, doctors can
improve treatment success rates.
- Treatment failures can be understood: Module
profiling can help doctors understand why treatments fail and switch to
more effective ones.
The future of skin care
The scientists hope that this
approach will be used in routine clinical practice in the future. It’s a move
towards a more personalised way of treating skin conditions, where decisions
are based on a deeper understanding of the individual patient’s unique biology.
This could mean quicker diagnoses and better outcomes for people struggling
with these conditions.
Journal information: https://www.nature.com/ncomms/
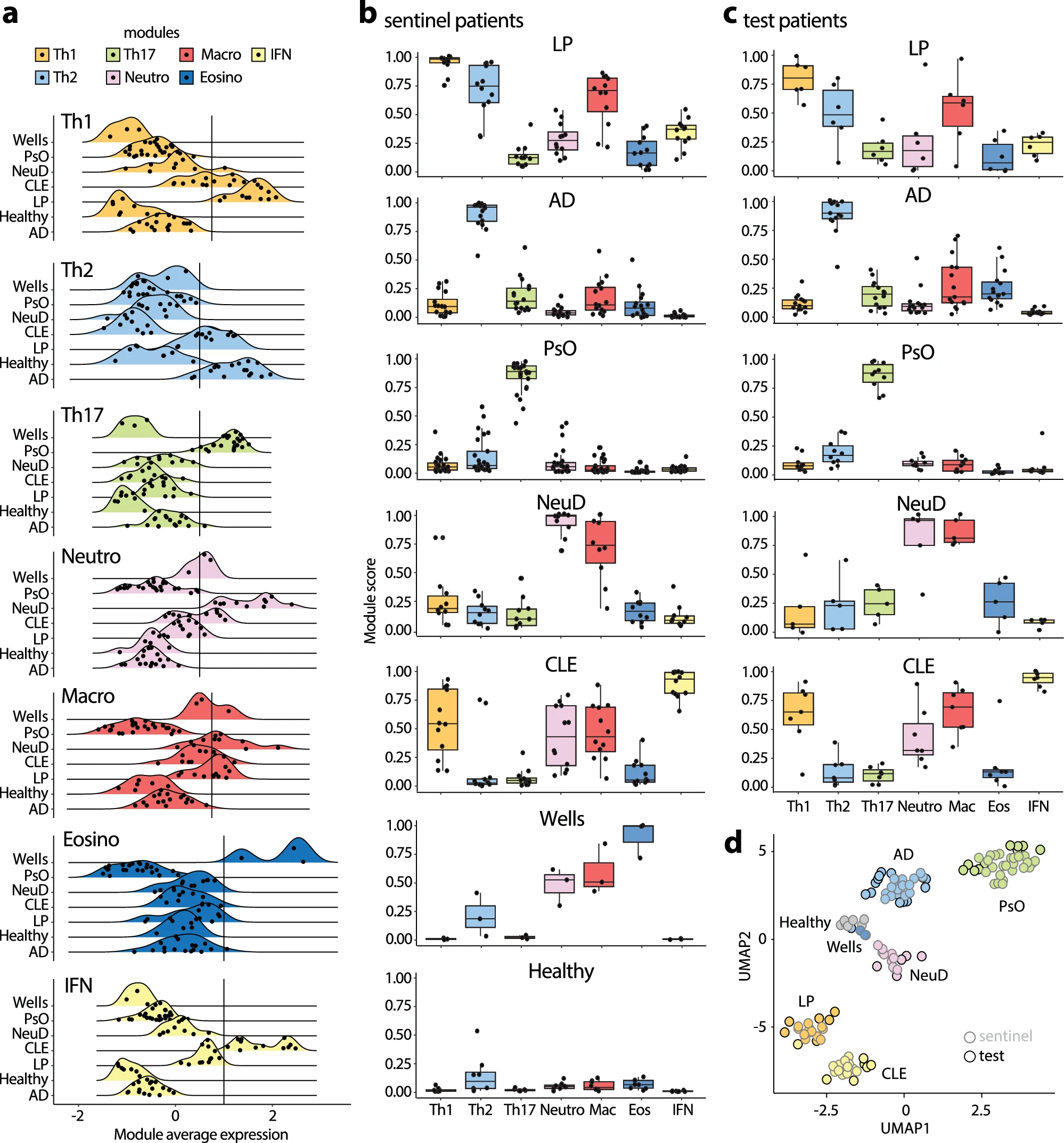



It is quite amazing to see the clear difference in picture a. Different skin diseases show their distinct immune modules. Though most skin conditions may not be fatal, the itchy feelings are really common and annoying. I also have eczema especially in dry winter and really hope there is a cure.
ReplyDeleteThank you for sharing your thoughts. It’s true that the immune system plays a fascinating role in distinguishing different skin diseases. The itchiness can indeed be very frustrating—I can relate to how tough it must be to deal with eczema, especially during the winter. Hopefully, advancements in research will bring us closer to a definitive cure soon!
ReplyDelete